Coronary Artery Disease

 Coronary artery disease (CAD), or ischemic heart disease, or is a disease where reversible or irreversible damage occurs to the heart muscle due to the restriction of blood flow. Coronary atherosclerosis is the major cause of CAD, rarely embolization of vegetation as in infectious endocarditis, embolization of calcifications in degenerative heart valve disease, arteritis, spasm and coronary artery dissection. It is the most common cause of death in developed countries, with the highest incidence in the older population - 80% of deaths are people over the age of 65.
Coronary artery disease (CAD), or ischemic heart disease, or is a disease where reversible or irreversible damage occurs to the heart muscle due to the restriction of blood flow. Coronary atherosclerosis is the major cause of CAD, rarely embolization of vegetation as in infectious endocarditis, embolization of calcifications in degenerative heart valve disease, arteritis, spasm and coronary artery dissection. It is the most common cause of death in developed countries, with the highest incidence in the older population - 80% of deaths are people over the age of 65.
Atherosclerotic plaques in the coronary artery wall cause stenosis which leads to myocardial ischemia. Stenoses above 70% are considered haemodynamically significant (except for the left main coronary artery, where stenosis of 50% is already considered significant). Smaller stenoses are not considered significant except during periods of increased work load - depending on the location, number and length of the stenosis. The clinical state, prognosis and therapy also depend on left ventricular function and the existence of possible collaterals.
Collaterals are branches of the coronary arteries that the body forms to bridge stenosis or occlusion in chronic CAD. There are homo-collaterals (some of the left / right coronary artery branches supply blood to stenosed branches of the same left / right coronary artery) and hetero-collaterals (anastomosis from the right coronary artery to the left, and vice versa).
Types of coronary artery disease
CAD may clinically manifest as chronic or acute disease. Chronic forms include stable angina, post-myocardial infarction, silent ischemia, chronic heart failure due to CAD, microvascular and vasospastic angina. Acute manifestations of CAD include unstable angina, acute myocardial infarction and sudden cardiac death.
| ACUTE CAD |
CHRONIC CAD |
| Unstable angina pectoris |
Stable angina pectoris |
| Acute myocardial infarction |
Status post myocardial infarction |
| Sudden cardiac death |
Chronic heart failure due to CAD |
| |
Vasospastic angina pectoris |
| |
Microvascular angina pectoris |
| |
Silent myocardial ischemia |
The term acute coronary syndrome (ACS) is often used in this context. It is a common term for acute types of ischemic heart disease - unstable angina and myocardial infarction. It was introduced for practical reasons - both are based on the rupture of an unstable atherosclerotic plaque and require immediate therapy. The difference is whether myocardial necrosis occurs or not. This may be distinguished by detection of subsequent washout of the cardio-specific enzymes in the blood.
STABLE ANGINA PECTORIS
Stable angina is a chronic condition arising from the existence of a narrowing atherosclerotic lesion in the coronary tree. Typical episodes of short reversible myocardial ischemia occur with increased oxygen demand - exertion, agitation, cooling. It is characterized by compressive to constricting chest pain, often associated with a shortness of breath. The pain is propagated to the left shoulder and upper limb, rarely to the neck, jaw, between the shoulder blades or to the epigastrium. The pain develops gradually and the intensity of the symptoms increases as the load continues. It resolves after stopping of exertion or after administration of nitroglycerin, usually within 5 minutes. If it does not disappear within 20 minutes, it is necessary to consider ACS.
The intensity of angina symptoms can be assessed according to the CCS (Canadian Cardiovascular Society) classification:
- Unlimited in normal daily activity. Difficulties only with maximum and prolonged workload
- Slight limitation of normal activities. Difficulties during increased workload - walking up the stairs> 1 floor, uphill, fast walking on levelled ground
- Significant reduction in routine activities. Difficulties during light workload – normal pace walking on levelled ground , up the stairs <1 floor
- Difficulties at rest or with minimal activity - walking around the apartment, etc.
STATUS POST MYOCARDIAL INFARCTION
It is a relatively wide group of patients - it includes patients who have been hospitalized for myocardial infarction in the past, as well as patients with retrospectively diagnosed heart attack (with the help of ECG or other options). Left ventricular post-infarction remodelling occurs. Its functional manifestations are hypokinesis (weakening of the contractile ability of the affected muscle area), akinesis (the affected area is virtually immobile) or dyskinesis (paradoxical, sometimes even aneurysmal ballooning of the thin fibrous scar). Patients may be completely asymptomatic or develop heart failure (see below). Ventricular dysrhythmias and thrombus embolism from post-infarct aneurysm are severe manifestations of chronic infarction but less common.
Unlike the healthy population, these patients require secondary atherosclerosis prevention with pharmacotherapy and life-style modifications. Surgical revascularization of the infarcted zone, especially scars, provides no significant benefit.
CHRONIC HEART FAILURE AS A RESULT OF CAD
Left ventricular dysfunction due to coronary artery disease. In some cases (e.g. diabetic patients who do not feel stenocardia because of neuropathy) this may be the first manifestation of CAD. Clinically it manifests as a shortness of breath, in severe cases as a pulmonary edema. The underlayment for dysfunction may be:
- Scar after myocardial infarction
- Aneurysm of the ventricular wall in the infarcted zone
- Papillary muscle dysfunction
- Mitral valve insufficiency (with altered geometry and dilatation of the left ventricule)
- Hibernated myocardium (see below)
Hibernated myocardium is a region of heart muscle with reduced contractility after repeated episodes of ischemia. It is a protective mechanism to prevent necrosis of heart tissue. In imaging studies, it is described as hypokinesis to akinesis of the specific segment. It can only be distinguished from scar by specific examinations (stress-dobutamine echocardiography, scintigraphy, magnetic resonance imaging). In case of successful revascularization of the hibernated myocardium, unlike scar tissue, function is gradually restored. As a result, hibernated myocardium is sometimes described as 'viable', which indicates the feasibility of revascularization procedures.
SILENT MYOCARDIAL ISCHEMIA
The clinical unit reserved for patients who are completely asymptomatic but have intermittent myocardial ischemia. They may have anatomically the same coronary involvement as in angina, however, they do not have chest pain. Ischemia is detected accidentally during stress test or Holter ECG monitoring. Asymptomatic ischemia is understood as a disturbed alarm mechanism, which is not limited to the myocardium alone, the cause is unclear. The absence of chest pain does not mean that the disease is less severe or that the ischemia is less extensive. Therefore the disease requires the same therapeutic procedures and life-style modifications as symptomatic angina pectoris.
Microvascular and vasospastic angina pectoris will not be discussed here in detail since cardiac surgery is not the treatment of choice there.
UNSTABLE ANGINA PECTORIS
The clinical condition resulting from atherosclerotic plaque rupture and subsequent intracoronary thrombosis. Myocardial necrosis does not occur and there are no elevated levels of cardiac enzymes. Here too, CCS classification is used to stratify clinical manifestations. These are:
- Newly emerging severe angina pectoris (at least grade CCS III)
- Sudden worsening of stable chronic angina by one degree (at least to CCS III)
- Episode of prolonged (> 20 min) resting stenocardia
ACUTE MYOCARDIAL INFARCTION
Acute myocardial infarction means acute ischemic necrosis of heart muscle due to the partial or complete occlusion of the coronary artery supplying that area. This happens mostly because of atherosclerotic plaque rupture and thrombosis. The diagnosis is based on clinical findings, ECG changes and laboratory findings - elevated blood cardiac enzymes levels. Clinically, it is important to distinguish between STEMI and NSTEMI.
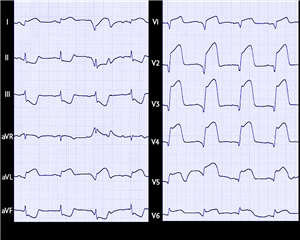 STEMI (ST- Elevation Myocardial Infarction) is a heart attack characterized by ST elevation on the ECG of at least 1mm in two adjacent leads. It usually means the complete closure of the proximal section of one of the coronary arteries and requires emergent transport to the catheterization laboratory to perform coronary angiography and PCI (percutaneous coronary intervention).
STEMI (ST- Elevation Myocardial Infarction) is a heart attack characterized by ST elevation on the ECG of at least 1mm in two adjacent leads. It usually means the complete closure of the proximal section of one of the coronary arteries and requires emergent transport to the catheterization laboratory to perform coronary angiography and PCI (percutaneous coronary intervention).
NSTEMI (Non-ST-Elevation Myocardial Infarction) is typically manifested on the ECG by ST segment depression and inversion of the T wave, but often there are no changes or the changes are less noticeable. It is caused by an incomplete coronary artery occlusion (acute significant stenosis), or by a more peripheral involvement. Coronary angiography is not emergently required, but is necessary for further patient management.
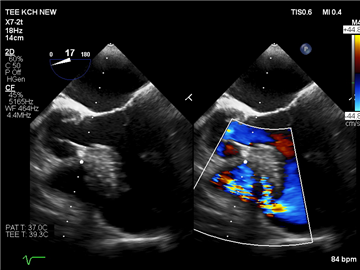
Mechanical complications of myocardial infarction. Severe myocardial infarction may cause serious conditions, often life-threatening, requiring immediate surgical treatment:
- papillary muscle rupture leading to acute mitral regurgitation
- rupture of the interventricular septum causing a left-right shunt
- left ventricular wall rupture leading to cardiac tamponade
- left ventricular wall rupture in a patient with adhesions between epicardium and pericardium (after inflammation, cardiac surgery…) leading to formation of pseudoaneurysm or bordered hemopericardium. It differs from aneurysm by a higher tendency to form thrombus, to cause heart failure, and by a higher risk of rupture. Histologically no cardiomyocytes can be detected in the pseudoaneurysm wall
Diagnosis and possible therapies of CAD
HISTORY AND PHYSICAL EXAMINATION
Information regarding chest pain (pressure or constrictive pain), often associated with the shortness of breath. It spreads to the left shoulder and left upper limb, rarely to the neck, jaw, between the shoulder blades or to the epigastrium. There may be association with exertion, agitation or cold. Especially in diabetics, the only manifestation is breathlessness - the so-called “anginal equivalent”.
In acute forms of coronary artery disease, this examination should focus only on the relevant information regarding the timing of events and the nature of the pain, eventually severe co-morbidities. It must not slow down the therapeutic process.
The physical findings of CAD are usually poor. In heart failure, the typical findings occur in the lungs (crackles in the bases, pulmonary edema).
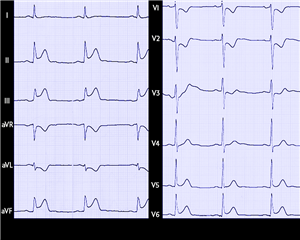
ELECTROCARDIOGRAPHY
The most basic examinations in CAD – typically ST-elevation or depression, flat or negative T-waves, pathological Q-wave (manifestation of post-infarction scar). In the case of a negative finding the diagnosis of CAD is not excluded, it is necessary to perform a stress test, most often ergometry.
A wide range of dysrhythmias, particularly atrial fibrillation or ventricular tachydysrhythmias, may occur. Nevertheless, they are not specific for CAD.
Ergometry is a stress ECG test that is performed when a patient is suspected to have CAD but the resting ECG shows no pathology. The patient connected to the ECG is exposed to gradual increases in physical load that can provoke myocardial ischemia with higher oxygen demand. The evidence of ischemia is newly developed ST depression.
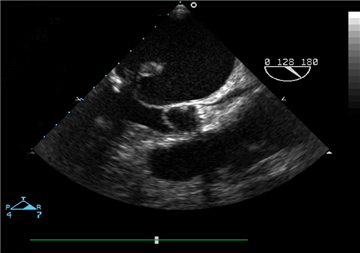
ECHOCARDIOGRAPHY
It is used to assess ventricular function, to assess local and general movement disorders (hypokinesis, akinesis, dyskinesis), to evaluate valve defects (ischemic mitral regurgitation), to detect mechanical complications of myocardial infarction. In hibernated myocardium it is important to perform a stress-dobutamine echocardiography.
Stress-dobutamine echocardiography focuses on comparing the resting echo-findings with the inotropic-dobutamine findings. In the hibernated regions the contractility is increased - this serves as an evidence of the viability of the affected myocardium and the meaningfulness of the revascularization procedures. The scar tissue does not respond to dobutamine.
OTHER EXAMINATIONS OF MYOCARDIAL VIABILITY
Single Photon Emission Computed Tomography (SPECT) using Thalium-201 or Technecium 99m radionuclides works by comparing the resting uptake of the radiopharmaceutical in the myocardium with peak uptake.
Magnetic resonance imaging using a paramagnetic contrast agent that is washed out very slowly from regions of acute myocardial infarction. Late-enhancement imaging sites correspond to areas of irreversible myocardial damage. Examination is also able to assess the transmurality of lesions - the larger the damage, the lower the chance of success with revascularization.
CORONAROGRAPHY AND CATHETERIZATION
It is an invasive examination which shows the coronary bed by injection of contrast medium directly into the right or left coronary artery. Currently it is an irreplaceable method for the detection and quantification of coronary artery stenosis. With the help of specific projections, it is possible to display all coronary arteries from multiple angles, on the left side:
- left main stem coronary artery (LMS)
- left anterior descending artery (LAD)
- diagonal branch (D)
- intermediate artery (IM)
- left circumflex artery (LCx)
- obtuse marginal branches (OM)
and on the right side:
- right coronary artery (RCA) and its branches:
- right posterolateral branch
- posterior descending artery (PDA)
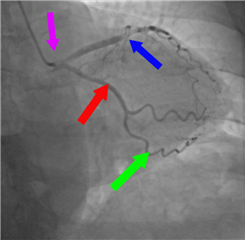
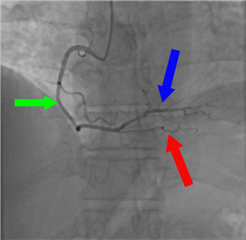
Coronarography is performed by a catheter inserted into the systemic vascular bed through the radial or femoral artery. The hemodynamic significance of stenosis is assessed by oculometry, in unclear cases additional tests are added to better quantify the stenosis:
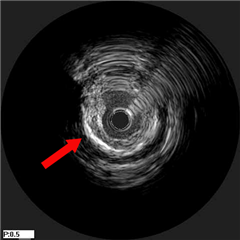 intravascular ultrasonography (IVUS) - sonographic imaging of the coronary artery lumen, it provides information not only about stenosis, but also about the structure of the vascular wall
intravascular ultrasonography (IVUS) - sonographic imaging of the coronary artery lumen, it provides information not only about stenosis, but also about the structure of the vascular wall- Fractional Flow Reserve (FFR) - measurement of the pressure difference before and after a stenosis at maximal coronary vasodilation (after adenosine administration). Currently the most recommended method of stenosis quantification, a stenosis is considered significant when the pressure ratio is <0.80.
- Instant wave-free ratio, iFR - measurement of pressure difference before and after a stenosis in the late phase of diastole when pulse waves are no longer present during the pressure measurement. Adenosine is not required. The results are prognostically comparable to FFR.
 Ventriculography - the imaging of the left ventricle by injecting a contrast medium directly into the ventricular cavity, provides an image of its global and regional contractility and also determines the ejection fraction of the left ventricle (physiologically above 60%).
Ventriculography - the imaging of the left ventricle by injecting a contrast medium directly into the ventricular cavity, provides an image of its global and regional contractility and also determines the ejection fraction of the left ventricle (physiologically above 60%).
CT-coronarography is a non-invasive variant of this examination. There is no need to introduce catheters, only intravenous contrast agent has to be administered. CT-derived FFR could be comparable to invasive FFR, but at present there is no widespread clinical adaption due to lack of valid data. The disadvantage of CT coronarography is the inability to immediately intervene in cases of severe stenosis in the ACS during the procedure. Therefore, classical invasive coronarography remains the gold standard for coronary artery assessment.
CAD TREATMENT OPTIONS
Drug therapy is the keystone of long-term disease control. All patients with CAD must take a 4-drug combination: acetylsalicylic acid, beta-blocker, ACE inhibitor and statin. For a transient period after an ischemic attack, a second anti-aggregant (clopidogrel or ticagrelor) is added (dual anti-aggregation). Antianginal drugs - nitrates and trimethazidine - are given in patients with angina. In heart failure, the patient receives diuretics, aldosterone antagonists, angiotensin receptor - neprilysin inhibitors, and other inotropics.
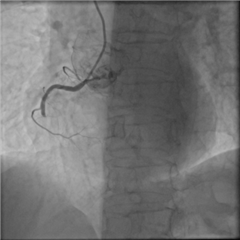
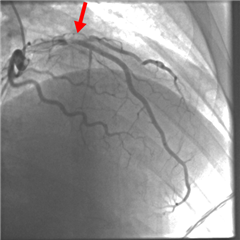
 Interventional treatment. Nowadays a very popular treatment option - percutaneous coronary intervention (PCI). Via the radial or femoral artery, a coronary angiography is performed and a stent is placed at the site of significant coronary stenosis. There it dilates the vessel and prevents restenosis. The risk of this procedure in the short-term is damage to the artery wall leading to dissection (in rare circumstances). In the long-term it is neoangiogenesis and consequently in-stent restenosis. We try to prevent this by implanting so-called drug eluted stent (DES) impregnated with a substance that prevents angiogenesis. The PCI method is irreplaceable in the treatment of acute coronary syndrome, particularly STEMI, and in the treatment of coronary lesions unsuitable for surgical therapy. A promising strategy is the use of PCI in hybrid revascularization. In rare cases, plain old balloon dilatation (POBA) of stenosis is done, at present it is almost phased out.
Interventional treatment. Nowadays a very popular treatment option - percutaneous coronary intervention (PCI). Via the radial or femoral artery, a coronary angiography is performed and a stent is placed at the site of significant coronary stenosis. There it dilates the vessel and prevents restenosis. The risk of this procedure in the short-term is damage to the artery wall leading to dissection (in rare circumstances). In the long-term it is neoangiogenesis and consequently in-stent restenosis. We try to prevent this by implanting so-called drug eluted stent (DES) impregnated with a substance that prevents angiogenesis. The PCI method is irreplaceable in the treatment of acute coronary syndrome, particularly STEMI, and in the treatment of coronary lesions unsuitable for surgical therapy. A promising strategy is the use of PCI in hybrid revascularization. In rare cases, plain old balloon dilatation (POBA) of stenosis is done, at present it is almost phased out.
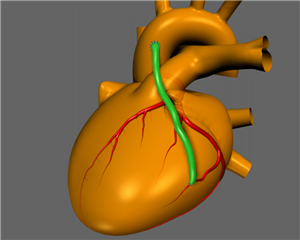
Surgical treatment. The principle of surgical treatment is bridging of coronary stenosis via bypass which will adequately supply the ischemic region of the myocardium with oxygenated blood. This procedure is termed surgical revascularization of the myocardium.
Indication for surgical revascularization
Indications for surgical myocardial revascularization are continuously being developed. This is mainly due to the development of interventional cardiology methods, in particular DES stents (high efficiency, good long-term outcome and low invasiveness) have taken over many of surgical indications. However, especially in younger patients with severe coronary disease, diabetes mellitus or left ventricular systolic dysfunction (left ventricular ejection fraction <50%), surgical revascularization remains irreplaceable - long-term results remain significantly better than those of interventional methods.
The SYNTAX score is used to assess the severity of the coronary lesions and choose the appropriate method of revascularization. It is an evaluation of angiographic finding, where each coronary artery stenosis gets a certain number of points according to its characteristics. If the total number of points is more than 22, the finding is considered severe and surgical revascularization is preferred.
The following indications for surgical revascularization are updated according to the latest guidelines of the European Society of Cardiology and the European Cardiothoracic Surgery Association (2018):
- Stable coronary artery disease: 3-vessel disease (LAD, LCx, RCA), left main stem disease, 2-vessel disease with proximal stenosis of LAD, 1-vessel disease (proximal LAD involvement must be present).
- NSTEMI: as with stable CAD but should be revascularized early. The only exception are patients in cardiogenic shock who need PCI on the lesion causing infarction (the so-called "culprit lesion"), other lesions are intervened on later.
- STEMI: absolutely preferred method is PCI for the culprit lesion, the remaining disease is taken care of in the second phase. Surgical revascularization is indicated only in case of unsuccessful PCI and continuing ischemia.
In case of other coronary involvement, the preferred choice is PCI or drug therapy. The strategies for surgical revascularization of the myocardium can be divided into 3 levels:
- Complete revascularization
- Hybrid revascularization
- Palliative revascularization
Complete revascularization stands for sewing a bypass on all significantly affected arteries with a diameter > 1.5 mm. The patient has the best long-term benefit from this strategy. The basic prerequisite is that the myocardial region supplied by the affected vessel remains viable. Revascularization of diffusely sclerotic arteries is questionable.
Hybrid revascularization is a combination of surgical and interventional techniques, mostly not simultaneously, independent of timing (surgery first and PCI second or vice versa). The aim of this method is to provide the patient with a bypass of LIMA on LAD, other lesions are treated by interventional techniques. It is used in patients with higher surgical risk, where we try to minimize operation time. Recently, there have been reports that a hybrid technique may have comparable long-term results with a classical revascularization strategy (Internal thoracic artery for LAD and venous grafts for remaining stenoses). The explanation may consist in technological advances and excellent long-term results of the new DES stents.
Palliative revascularization (especially palliative MIDCAB) is a method of incomplete revascularization in complex coronary involvement in high-risk patients.
Principles of surgical revascularization
The aim of revascularization procedures is to bring enough oxygenated arterial blood to ischemic regions of the myocardium (beyond the stenotic lesion or coronary artery occlusion). This is achieved by bridging, bypass. Two types of grafts can be used for bypass surgery:
- Venous: great saphenous vein (GSV) or lesser saphenous vein
- Arterial: left or right internal thoracic/mammary artery (LIMA, RIMA), radial artery (RA), right gastroepiploic artery (RGEA) or inferior epigastric artery


These vessels can be used as free grafts - after preparation, the vein or artery is cut at the proximal and distal end, the distal end is connected to the coronary artery in the form of end-to-side anastomosis, the proximal end is anastomosed to the ascending aorta in an end-to-side fashion. This is known as an aorto-coronary bypass.
Some arteries can also be used as an in-situ graft - the surgeon cuts only the distal end of the artery and re-connects it to the coronary artery. This is mostly performed on LIMA or RIMA graft – mammaro-coronary bypass; RGEA may be used in this fashion, too.
 The gold standard in coronary surgery is an in-situ LIMA on RIA and free venous grafts (GSV) on the remaining significantly affected coronary arteries. LIMA is generally considered the best graft because its 10-year patency is 90-95%. For reference only, venous grafts have a 10-year patency of 50-60%. In recent years, arterial polygrafting, or even total arterial revascularization, has become very popular. It is a strategy where arterial grafts are used preferentially or exclusively. When anastomosed to severely stenotic coronary vessels, there is a significant benefit over venous grafts in patency, patient survival, risk of heart attack or need for extra revascularization procedures after 5 years.
The gold standard in coronary surgery is an in-situ LIMA on RIA and free venous grafts (GSV) on the remaining significantly affected coronary arteries. LIMA is generally considered the best graft because its 10-year patency is 90-95%. For reference only, venous grafts have a 10-year patency of 50-60%. In recent years, arterial polygrafting, or even total arterial revascularization, has become very popular. It is a strategy where arterial grafts are used preferentially or exclusively. When anastomosed to severely stenotic coronary vessels, there is a significant benefit over venous grafts in patency, patient survival, risk of heart attack or need for extra revascularization procedures after 5 years.
 Sequential bypass. By default, one graft is used to bypass the stenosis of one coronary vessel in an end-to-side fashion, this is known as a "single" bypass. However, the sequential bypass method uses a single graft to revascularize multiple coronary arteries. The terminal, or distal anastomosis is a standard end-to-side. In addition, side-to-side anastomoses are sewn along the graft. Thus, for example, IM + OM1 + OM2 or LAD + D1 can be revascularized with a single graft. Despite initial concerns about the use of sequential bypasses (fear of extensive ischemia in the case of a proximal graft closure), these grafts have been shown to have significantly better long-term outcomes in terms of mortality, heart attack, or graft occlusion. The reason is probably higher flow in sequential bypass, which prevents intimal proliferation and stenosis.
Sequential bypass. By default, one graft is used to bypass the stenosis of one coronary vessel in an end-to-side fashion, this is known as a "single" bypass. However, the sequential bypass method uses a single graft to revascularize multiple coronary arteries. The terminal, or distal anastomosis is a standard end-to-side. In addition, side-to-side anastomoses are sewn along the graft. Thus, for example, IM + OM1 + OM2 or LAD + D1 can be revascularized with a single graft. Despite initial concerns about the use of sequential bypasses (fear of extensive ischemia in the case of a proximal graft closure), these grafts have been shown to have significantly better long-term outcomes in terms of mortality, heart attack, or graft occlusion. The reason is probably higher flow in sequential bypass, which prevents intimal proliferation and stenosis.
Jumping bypass is a simmilar technique, the difference is that multiple anastomoses of one graft bridge significant stenosis of only one coronary artery, most often LAD.
 A composite bypass is another possible variation of bypass techniques. In this technique, another venous or arterial graft is anastomosed to another venous or arterial graft in the shape of the letter “Y” or “T” and used to revascularize other regions of the myocardium. As with sequential bypass, this technique leads to increased graft flow, which in the long run may decrease the risk of occlusion. Sequential and composite bypasses are most often used in significant atherosclerotic involvement of the aorta (we reduce or eliminate the need for aortic cross-clamping), or when the grafts are too short or insufficient, or when attempting total arterial revascularization.
A composite bypass is another possible variation of bypass techniques. In this technique, another venous or arterial graft is anastomosed to another venous or arterial graft in the shape of the letter “Y” or “T” and used to revascularize other regions of the myocardium. As with sequential bypass, this technique leads to increased graft flow, which in the long run may decrease the risk of occlusion. Sequential and composite bypasses are most often used in significant atherosclerotic involvement of the aorta (we reduce or eliminate the need for aortic cross-clamping), or when the grafts are too short or insufficient, or when attempting total arterial revascularization.
Procedures in surgical myocardial revascularization
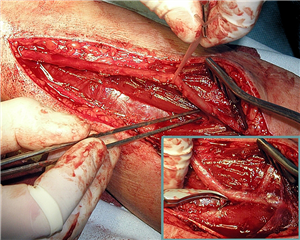
The standard procedure for surgical revascularization of the myocardium begins with opening of the chest cavity through a median sternotomy approach. The planned grafts are harvested for revascularization (LIMA, RIMA, the assistant surgeon also harvests GSV or RA grafts).
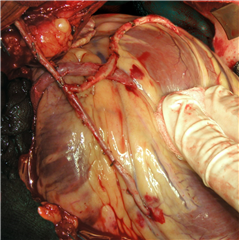
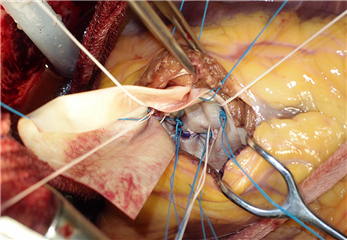
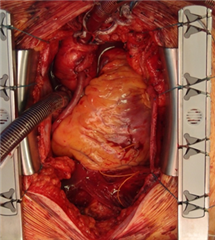 The on-pump coronary artery bypass grafting (on-pump CABG) using extracorporeal circulation is considered the gold standard for surgical revascularization of the myocardium. After harvesting the grafts, cannulas for extracorporeal circulation are introduced, followed by cross-clamping of the ascending aorta and administration of cardioplegic solution. In the non-beating heart distal anastomoses of bypasses are performed on the corresponding coronary vessels. After the distal anastomoses are done, the aortic clamp is released, the heart begins to beat again, and during this period the proximal anastomoses of the free grafts are performed on the ascending aorta. The extracorporeal circulation is then terminated, and the chest is closed.
The on-pump coronary artery bypass grafting (on-pump CABG) using extracorporeal circulation is considered the gold standard for surgical revascularization of the myocardium. After harvesting the grafts, cannulas for extracorporeal circulation are introduced, followed by cross-clamping of the ascending aorta and administration of cardioplegic solution. In the non-beating heart distal anastomoses of bypasses are performed on the corresponding coronary vessels. After the distal anastomoses are done, the aortic clamp is released, the heart begins to beat again, and during this period the proximal anastomoses of the free grafts are performed on the ascending aorta. The extracorporeal circulation is then terminated, and the chest is closed.
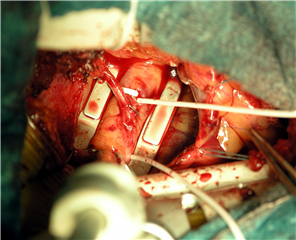
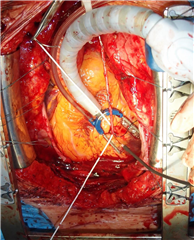 Alternatively, myocardial revascularization can be achieved without the use of extracorporeal circulation. This is known as off-pump coronary artery bypass grafting (OPCAB). The keystone for achieving this is local stabilization of the region where the surgeon plans to place the distal anastomosis. This is achieved with the help of a special stabilization system, which uses pressure or suction to stabilize the epicardium around the target artery and thus allows microanastomosis. Bloodlessness of the surgical field is achieved by the use of intracoronary shunt, temporary coronary artery occlusion using a silicone stitch and “blowing” blood out of the field using carbon dioxide “blower”. At the same time, it is necessary not to compromise cardiac activity during operation, because the blood circulation is dependent on patient’s heart function throughout the operation.
Alternatively, myocardial revascularization can be achieved without the use of extracorporeal circulation. This is known as off-pump coronary artery bypass grafting (OPCAB). The keystone for achieving this is local stabilization of the region where the surgeon plans to place the distal anastomosis. This is achieved with the help of a special stabilization system, which uses pressure or suction to stabilize the epicardium around the target artery and thus allows microanastomosis. Bloodlessness of the surgical field is achieved by the use of intracoronary shunt, temporary coronary artery occlusion using a silicone stitch and “blowing” blood out of the field using carbon dioxide “blower”. At the same time, it is necessary not to compromise cardiac activity during operation, because the blood circulation is dependent on patient’s heart function throughout the operation.
The OPCAB method has gained popularity mainly for 2 reasons:
- Minimizing manipulation with the ascending aorta (and thus reducing the risk of atherosclerotic material being released from the aortic wall and subsequent stroke)
- Minimizing patient blood contact with foreign surfaces of extracorporeal circulation tubes (reducing systemic inflammatory response)
Recent studies, however, show that there is significant difference neither in perioperative nor in long-term risk between “on-pump” and “off-pump” procedures. Due to higher technical demands and results of these studies, the OPCAB method is currently in decline. It retains its place in revascularization of patients with severe atherosclerosis of the ascending aorta (porcelain aorta) or in patients with severe co-morbidities.
Minimally invasive direct coronary artery bypass grafting (MIDCAB) is a method that combines the benefits of revascularization without the use of extracorporeal circulation with minimally invasive surgical approach. The procedure is performed through a small left-sided thoracotomy in the 4th or 5th intercostal space. After LIMA harvest, the LAD bypass is performed using the off-pump technique. In comparison to standard cardiac surgical procedures, the method yields little operative burden for the patient and offers the best of coronary surgery at the same time - bypass of LIMA to LAD, which has the best long-term results of all. This technique is popular not only as a causal complete therapy for solitary involvement of LAD, but also as a part of a hybrid or palliative revascularization (see above).
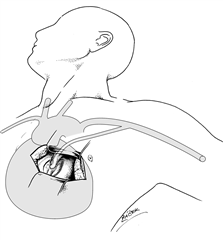
TECAB (totally endoscopic coronary artery bypass grafting) is an alternative to classical MIDCAB, where the entire operation is conducted using endoscopic instruments through ports in the thoracic wall under camera control. The highest level of miniinvasivity resides in robotic technology (or telemanipulation) where the LIMA harvest or even the whole surgery is performed remotely using robotic arms on a beating / stopped heart.
Additional procedures in surgical therapy of CAD
They are usually combined with standard surgical myocardial revascularization.
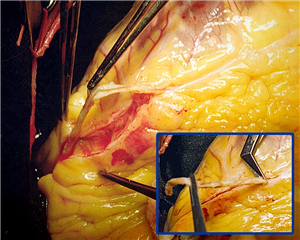 Endarterectomy is a surgical procedure useful in an attempt to revascularize a coronary artery that is almost or completely obliterated due to atherosclerosis. It means removing a large atheromatous plaque from the coronary artery around the site of incision. A graft is then sutured to the renewed lumen of the coronary artery. It may be a planned procedure for complete revascularization, but most surgeons perform it only when there is no other choice (when a coronary artery lumen is found to be more severely occluded than expected by coronarography). At present, this technique is rarely used and is performed only at experienced workplaces.
Endarterectomy is a surgical procedure useful in an attempt to revascularize a coronary artery that is almost or completely obliterated due to atherosclerosis. It means removing a large atheromatous plaque from the coronary artery around the site of incision. A graft is then sutured to the renewed lumen of the coronary artery. It may be a planned procedure for complete revascularization, but most surgeons perform it only when there is no other choice (when a coronary artery lumen is found to be more severely occluded than expected by coronarography). At present, this technique is rarely used and is performed only at experienced workplaces.
Transmyocardial Laser Revascularization (TMLR) is different from the standard direct revascularization procedures. In this technique the blood is delivered to the ischemic myocardium via extraanatomical communications from the left ventricle cavity. Communications (narrow channels) are generated by laser beam pulses directed from the epicardium to the left ventricle cavity. The beneficial effect of this procedure is most often explained by inflammatory neoangiogenesis in the vicinity of the canal, partialy also by the denervation of ischemic muscle. Symptomatic improvement in severe angina pectoris (CCS IV) can be achieved with TMLR in patients, in whom optimal medical therapy is insufficient and no direct revascularization intervention can be performed. However, the effect on overall survival has not been demonstrated.
Correction of ischemic mitral regurgitation. The morphological basis of ischemic mitral regurgitation is the partial or complete ischemic rupture of the papillary muscle (acute mitral insufficiency), or papillary muscle dysfunction or annular dilation in left ventricular post-infarction dysfunction (chronic mitral insufficiency). Surgical correction is bound with high mortality, particularly in the acute phase. The gold standard is the replacement of the mitral valve. In some cases, it is possible to preserve the valve and perform a plasty.
 Postinfarction ventricular septal defect closure. An acute left-to-right shunt is always haemodynamically significant and leads to severe deterioration of blood circulation, often leading to cardiogenic shock and death. The condition requires both pharmacological and mechanical circulation support, followed by surgical correction. The timing of the operation is problematic - in patients with uncontrollable shock it is essential to proceed immediately with surgery and close the defect with a patch. However, placing the patch in the surrounding necrotic myocardium is technically demanding and risky. If the operation can be postponed for 2-3 weeks, the edges of the defect become fibrous and surgical correction is relatively safer.
Postinfarction ventricular septal defect closure. An acute left-to-right shunt is always haemodynamically significant and leads to severe deterioration of blood circulation, often leading to cardiogenic shock and death. The condition requires both pharmacological and mechanical circulation support, followed by surgical correction. The timing of the operation is problematic - in patients with uncontrollable shock it is essential to proceed immediately with surgery and close the defect with a patch. However, placing the patch in the surrounding necrotic myocardium is technically demanding and risky. If the operation can be postponed for 2-3 weeks, the edges of the defect become fibrous and surgical correction is relatively safer.
Resection of the left ventricular aneurysm leads to an improvement of geometric shape of the left ventricle and to an increase in the overall ejection fraction. The prerequisite for a successful procedure is a sufficient amount of well-preserved cardiac muscle from which it is possible to reconstruct the left ventricular cavity.
Closure of postinfarction rupture of the left ventricular wall. It is a serious complication of acute myocardial infarction and almost always results in death (in cardiac tamponade). If an immediate transfer of the patient to the operating room can be managed, a surgical treatment can be attempted, but the suture of the necrotic muscle of the left ventricular wall is extremely difficult.
Resection of the left ventricular pseudoaneurysm. Left ventricular pseudoaneurysm is indicated for surgical treatment because of the risk of rupture, embolism and heart failure. The principle of the operation is the preparation of the pseudoaneurysm sac, its removal and closure of the communication with the left ventricular cavity.
RESULTS
The early mortality of surgical myocardial revascularization is about 2% on average. It is lower in planned interventions, in patients with good ejection fraction and without major comorbidities. On the other hand, it increases with age, left ventricular dysfunction, diabetes, chronic obstructive pulmonary disease, renal insufficiency, atherosclerosis of cerebral or peripheral arteries.
In the long term, if surgical revascularization is performed in well-indicated cases, it has been shown to significantly reduce long-term mortality, the risk of further myocardial infarction and the need for re-do revascularization compared to interventional methods or pharmacological treatment.
Resources:
- Češka R a kol. Interna. Praha: Triton, 2010. ISBN: 978-80-7387-423-0.
- Dominik J. Kardiochirurgie. Praha: Grada Publishing, 1998. ISBN: 80-7169-669-2.
- Gwozdziewicz M. Arteriální revaskularizace myokardu. Praha: Grada 2007. ISBN: 978-80-247-1772-2.
- Neumann FJ, Sousa-Uva M, Anders A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularizationi. European Heart Journal 2019; 40 (2): 87-165, https://doi.org/10.1093/eurheartj/ehy394
- Vojáček JF. iFR a FFR - současné možnosti stanovení funkční významnosti koronární stenózy. Intervenční a akutní kardiologie 2018; 17 (2): 62-65.
- Cohn LH, Adam DH. Cardiac Surgery in the Adult, Fifth Edition. New York: McGraw Hill Education, 2016. ISBN 978-0-07184487-1.
- Klener P, et al. Vnitřní lékařství - Čtvrté, přepracované a doplněné vydání. Praha: Galén, 2015. ISBN: 978-80-7262-705-9.
- Dominik J.: Kardiochirurgie. In.: Pafko P. et al.: Základy speciální chirurgie, Galén, 2008, s.173-195. ISBN 978-80-7262-402-7
- Harrer J.: Chirurgická léčba ischemické choroby srdeční. In.: Vojáček J., Kettner J.: Klinická kardiologie, IV.vyd., Maxdorf, 2019, s.208-226. ISBN 978-80-7345-600-9
